Is a syndrome defined by chronic widespread pain of at least 6 months in duration. It is a multisystem disease associated with neurological and psychological symptoms including nonrefreshive sleep, fatigue, anxiety, depression and cognitive disfunctions. The cause of fibromyalgia is not cleared yet and is still debatable. Available evidence implicates the CNS as key in maintaining pain such as the other symptoms of fibromyalgia.
According to the 1990 American College of Rheumatology criteria , a patient must have pain in the axial skeleton, pain at the level above and bellow the waist, and pain during palpation in at least 11 to 18 paired tender ponts through whole body. The majority of patients(80%) are women. Prevalence of the disease increases by age and is reater about 10% more in women older than 60 years.
SYMPTOMATOLOGY
Fibromyalgia is characterized by widespread and longlasting pain more than 3 months in the presence of tender points at specific anatomic sites. A series of other symptoms are frequently present. These include marked fatigue, stiffness, sleep disorders, cognitive disturbances, psychological distress, temporomandibular joint syndrome, paresthesias, headache, genitourinary manifestations irritable bowel syndrome, and orthostatic intolerance.
PHYSICAL EXAMINATION
The findings of the general medical and neurologic examinations should be normal. Blood pressure recording for orthostatic hypotension is performed. Mood and affect are noted. The tender points are palpated with approximately 4kg/cm2 of pressure. This is just enough pressure to blanch (a temporary whitening of the skin due to transient ischemia) the fingernail of the examiner.The patient will experience pain at these locations.
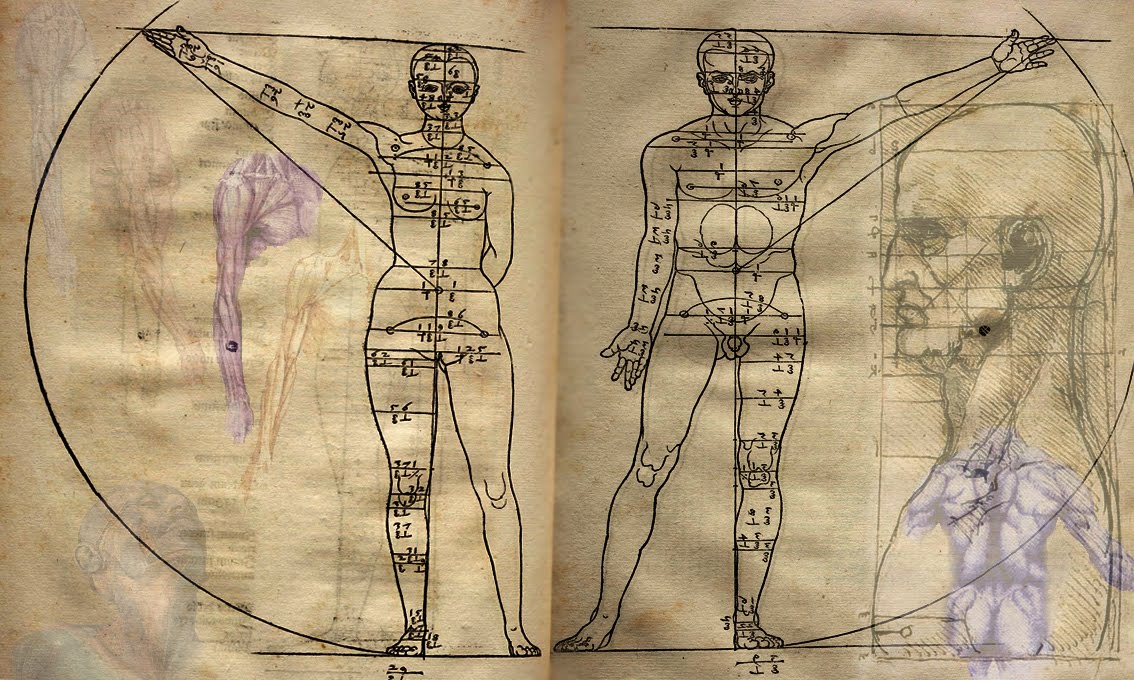
 Locations of the 18 tender points of fibromyalgia.
Locations of the 18 tender points of fibromyalgia.In addition, a comprehensive neurologic and musculoskeletal examination is performed to rule out superimposed pain generators, such as bursitis, tendinitis, radiculopathy, and myofascial trigger points.
FUNCTIONAL LIMITATION OF THE FM
Patients are limited in their ADL's and exercise tolerance by both pain and fatigue. Patients report also cognitive dysfunctions with difficulty in concetration, organization, and motivation. This is known as ''Fibro Fog''. About 25% of patients with fibromyalgia report themselves disabled and are collecting some form or disability payment. Individuals are more likely to become disabled if they report higher pain scores, work at a job that requires heavy physical labor, have poor coping strategies and feel helpless, or are involved in litigation.
DIAGNOSTIC METHODS
FB is a clinical diagnosis. For other conditions to be excluded, basic laboratory tests may be appropriate, such as complete blood count, erythrocyte sedimentation rate, thyroid stimulating hormone concentration, and creatinine kinase activity. Primary sleep disorders may need to be identified by sleep studies. Radiography or MRI may be indicated if osteoarthritis, radiculopathy, spinal sclerosis, or intrisic joint disease is suspected or even overshadowed. Electrodiagnostic studies maybe usefull if entrapment neuropathy or radiculopathy is suspected.
DIFFERENTIAL DIAGNOSIS
Thyroid myopahty
Metabolic myopathy
Mood disturbances
Somatoform pain disorders
TREATMENT
Initial Treatment includes education of the patient, pharmacologic treatment, gentle exercises and relaxation training. Education of the patient includes individual and group classes that review the symptoms of fibromyalgia; it reassures the patient as to the generally bening course and outlines the treatment path.
Pharmacologic management has as primary goal to normalize sleep dsorders and to diminish pain. Low dose tricyclic anti-depressants at bedtime (e.g.amitriptyline, 10 to 20 mg) with low dose selective serotonin reuptake inhibitors (e.g. fluoxetine,20 mg every morning) is a promissive combination. The combination works better than either medication alone. Studies demonstrate that treatments affecting levels of norepinephrine and serotonin have the greates impact on important symptoms, including pain and sleep.
The serotonin-norepinephrine reuptake inhibitors venlafaxine and duloxetine demonstrate benefit in patients with fibromyalgia.
Pain may be relieved with simple analgetics, such as acetaminophen or NSAIDS. Tramadol is the next-line agent. Pregabali, a newer anticonvulsant, reduces pain in patients with FB at doses of 300-450 mg /day, starting with 50mg three times daily and increasing to 100mg trhee times daily durin one week (7 days). Opioids are rarely used. Adjunctive nonpharmacologic pain control methods include acupuncture, massage, and biofeedback.
REHABILITATION
Physical Therapy is used to educate the patient in a stratching, gentle strengthening and cardiovascular fitness program. This can improve fitness and function, and decrease pain. Occupational therapy is incorporated to review ergonomics of daily activities, and activities of daily living are reviewed at the work site. Task simplification, pacing and maximization of function are emphasized.
Mental health professionals can be helpful in the rehabilitative phase tp educate the patients in a mind-body positive coping strategies for living with chronic pain. Associated depressionand anxiety often need psycho-pharmacologic treatment as well.
A stepwise approach to fibromyalgia management is recommended. The first step is to confirm the diagnosis, to explain the condition, and to treat any comorbid illness, such as mood or sleep disturbance.
The second step is to try a low dose tricyclic antidepressant or cyclobenzaprine. The patient should begin a cardiovascular exercise program and be refferred for congnitive behavioral therapy or combine that with exercise.
The third step includes specialty referral (i.e., rheumatology,physiatry, psychiatry, pain management), Trials with selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors or tramadol should be considered. One may use a combination medication trial or anticonvulsant.
PROCEDURES
Trigger Point Injections
Myofascial trigger points may be injected with 1% lidocaine to decrease local pain. Patients with recalcitrant chronic myofascial pain may respond to injections with botulinum toxin.
If patients have concurrent bursitis, tendinitis, or nerve entrapment, therapeutic injections may be performed to treat these specific diagnoses.
Acupuncture
Acupunture can be used for treatment of pain and fatigue. Preliminary studies suggest that the benefit may last up to several months. Treatment one or two times per week for at least 6 visits appears necessary. Improvement lastas at least 1 month but is likely to waneover time e.g 6 months. The optimal number and frequency of acupuncture treatments have not been determined.
ELECTROTHERAPY
Electrotherapy, including transcutaneous electrical stimulation (TENS), electro-acupuncture, functional electrical stimulation, iontophoresis, laser interferential therapy and ultrasound, has been used in musculoskeletal pain conditions. Interferential electrotherapy with amplitude modulated at low frequencies reaches deep muscles and nerves, stimulates voluntary muscles, promotes an increase in peripheral
blood flow, accelerate bone healing and reduces pain.
Besides different sites of action, the combination of electrical therapy and ultrasound is more effective than each of them separately because it provides localised analgesia on previous detected painful areas.
ULTRASOUND
Ultrasound therapy has achieved recognition as a suitable method in physical medicine in treatment of acute and chronic musculoskeletal disorders. Experimental studies have shown that it is possible to heat deeper structures, such as joints, muscle and bone, with ultrasound.Although muscular pain has been a central feature of FM syndrome, controlled studies are controversial in supporting a role for muscle in pathophysiology of this condition.
Perfusion and metabolic changes have been proposed to explain focal sustained contraction as well as, muscle deconditioning. Pulse ultrasound therapy improves sustained muscle contraction by increasing the permeability of the cell membrane; improves intracellular energy consumption;
increases angiogenesis in ischemic tissues repair.r. In a recent study suggest that combined therapy
with pulsed ultrasound and interferential current, acting as an electrodiagnostic tool and as modality of physical therapy, provides an effective pain treatment, with consequent sleep improvement in FM.
TRANSCUTANEOUS ELECTRICAL NERVE
STIMULATION (TENS)
TENS is the most common example of electrically based analgesia. A satisfactory explanation of the mechanisms of TENS analgesia does still not exist. Recent research has proposed that TENS also stimulates the sympathetic nervous system and brain stem nuclei to produce endorphins and may inhibit arthritis related inflammation. Pain is the most common indication for TENS. Success rates in clinical studies vary from lows of about 25% to highs of about 80 to 95% and may be affected by a variety of different factor.
Since FM is characterised by generalised musculoskeletal pain, it is obvious that the use of TENS is limited.
Nevertheless in some cases were a localised musculoskeletal pain problem is prominent the use of TENS is certainly justified based on the available clinical data in other conditions. A major advantage of TENS is its applicability to a home program and patient control of the treatment schedule. The effectiveness of TENS depends on proper instruction and monitoring of its use.
Specifically in FM, electroanalgesia by TENS and electro-acupuncture has been used with controversial results.
POTENTIAL DISEASE COMPLICATIONS
Failure to make the diagnosis early may lead to delay in treatment, deconditioning, and expensive unnecessary medical testing and procedures. Chronic, intractable pain may occur despite treatment.
POTENTIAL TREATMENT COMPLICATIONS
Tricyclic antidepressant medications can be associated with anticholinergic side effects, such as urinary retention, sedation, constipation and weight gain. Selective serotonin reuptake inhibitor medications may be associated with sexual dysfuntion, gastrointestinal intolerance, and anorexia. Overly aggressive exercise programs may transiently increase pain in some patients. Local injections may result in local pain, ecchymosis, intravascular injection, or pneumothorax if they are improperly executed. There is an increased risk of bleeding with use of NSAIDS or selective serotonin reuptake inhibitors. For patients taking high dose of serotonin reuptake inhibitors consider avoidance or minimal use of NSAIDS. The threshold for seizures is lowered by tramadol. In addition the risk of seizures is enhanced by the concomitant use of tramadol with selective serotonin reuptake inhibitors.
Walter R Frontera, Julie K Silver, Thomas D. Rizzo, Essentials of Physical Medicine and Rehabilitation, musculoskeletal disorders, pain,and rehabilitation, second edition. Saunders Elsevier 2008 ISBN: 978-1-4160-4007-1




No comments:
Post a Comment